A sacroiliac (SI) joint injection—also called a sacroiliac joint block—is primarily used either to diagnose or treat low back pain and/or sciatica symptoms associated with sacroiliac joint dysfunction.
Watch:Sacroiliac Joint Steroid Injection Video
The sacroiliac joints lie next to the spine and connect the sacrum with the hip on both sides. There are two sacroiliac joints, one on the right and one on the left. Joint inflammation and/or dysfunction in this area can cause pain.
Read more about Sacroiliac Joint Dysfunction.
The purpose of a sacroiliac joint injection is two-fold: to diagnose the source of a patient's pain, and to provide therapeutic pain relief. At times, these are separated and a patient will undergo a purely diagnostic or therapeutic injection, although often the two are combined into one injection.
- Injected medicines are commonly used in healthcare settings for the prevention, diagnosis, and treatment of various illnesses. Unsafe injection practices put patients and healthcare providers at risk of infectious and non-infectious adverse events and have been associated with a wide variety of procedures and settings.
- If this second diagnostic injection also provides 75-80% pain relief for the duration of the anesthetic, there is a reasonable degree of medical certainty the sacroiliac joint is the source of the patient's pain.
Be attentive to the long description of the HCPCS code. The definition of the HCPCS code specifies the lowest common denominator of the amount of dosage. Use the units' field as a multiplier to arrive at the dosage amount. For example, J1756 is an injection for iron sucrose, 1 mg for a total dosage of 100 mg; report 100 in the units' field. References 1 Mittal et al Transthoracic cardioversion of atrial fibrillation. 2000;101:1282-1287 2 Niebauer et al Cardioversion thresholds of atrial fibrillation and atrial flutter using an external biphasic waveform defibrillator. Presented at NASPE 2000 (abstract) 3 Friedman et al Role of ibutilide and biphasic waveforms for cardioversion of atrial fibrillation in.
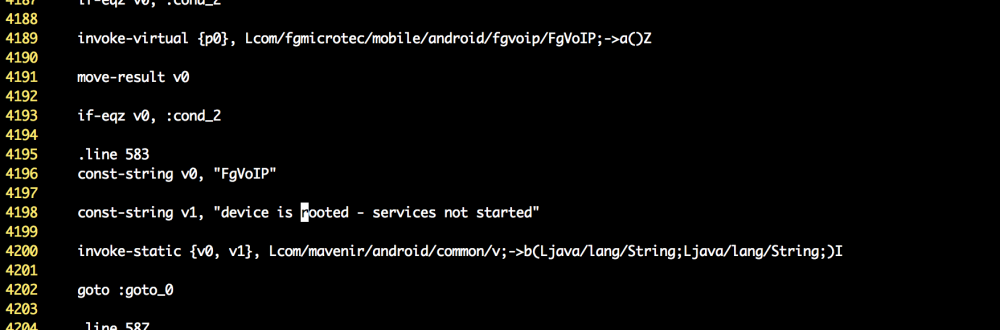
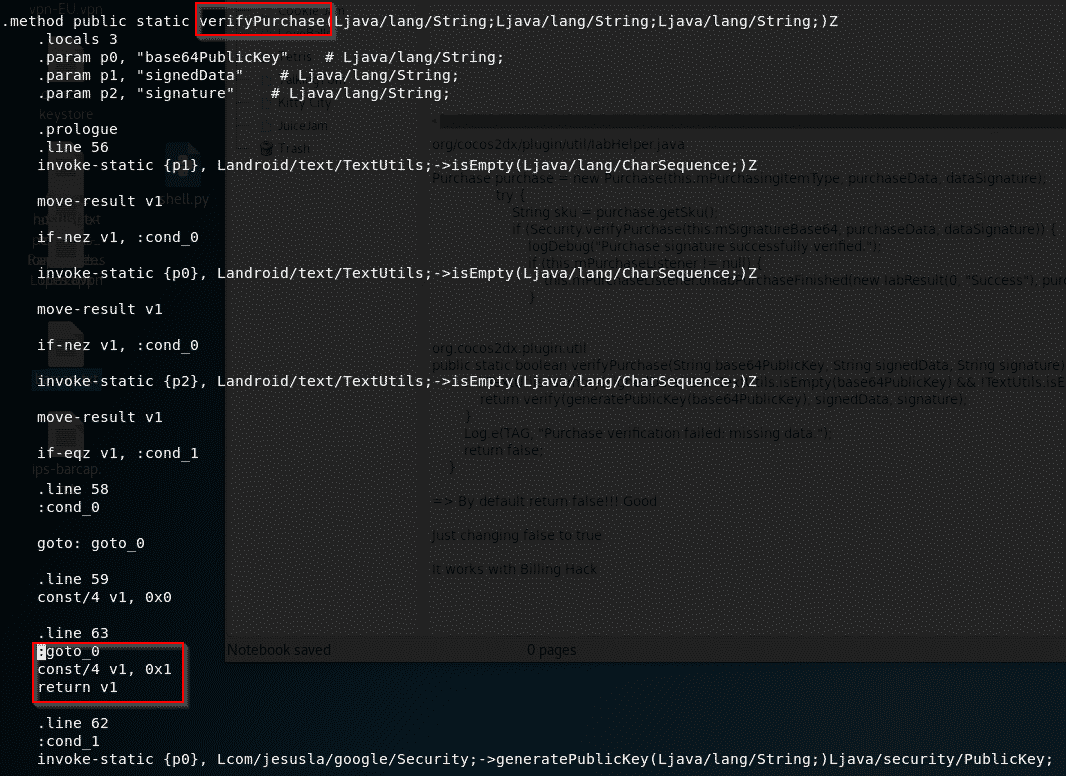
Smali Syntax
Diagnosis
A diagnostic SI joint injection is used to confirm a suspected diagnosis of sacroiliac joint dysfunction. This is done by numbing the sacroiliac joint with local anesthetic (e.g. lidocaine). The injection is performed under fluoroscopy (X-ray guidance) for accuracy. Once the needle has entered the sacroiliac joint, contrast is injected into the joint to ensure proper needle placement and proper spread of medication. The numbing medication is then injected into the joint.
After the numbing medication is injected, the patient is asked to try and reproduce the pain by performing normally painful activities. If the patient experiences 75-80% pain relief for the normal duration of the anesthetic, a tentative diagnosis of SI joint dysfunction is made. A second diagnostic sacroiliac injection should be performed using a different numbing medication (e.g. Bupivicaine) in order to confirm the diagnosis.
If this second diagnostic injection also provides 75-80% pain relief for the duration of the anesthetic, there is a reasonable degree of medical certainty the sacroiliac joint is the source of the patient's pain.
Some practitioners are performing lateral branch blocks to diagnose SI joint pain. The lateral branch nerves are small nerves that branch off the sacral spinal nerves and provide sensation to the joint. A lateral branch block might be performed to determine if a patient is a candidate for a radiofrequency nerve ablation to provide longer lasting relief of the pain associated with SI joint dysfunction.Pain Relief
A therapeutic SI joint injection is done to provide relief of the pain associated with sacroiliac joint dysfunction. The injection is performed using the same technique as a diagnostic SI joint injection, except that anti-inflammatory medication (corticosteroid) is included in the injection to provide pain relief by reducing inflammation within the joint.
If the patient experiences prolonged pain relief after a therapeutic sacroiliac joint injection, he or she can begin a physical therapy and rehabilitation program to further reduce pain and return the patient to normal activity levels.
If the therapeutic sacroiliac joint injection is successful in reducing or eliminating the patient's pain for a longer duration, it may be repeated up to three times per year, in conjunction with physical therapy and rehabilitation program, to help the patient maintain normal function.
The Sacroiliac Joint Injection Procedure
The Sacroiliac Joint injection procedure is usually performed in an operating room or a dedicated procedure room. The entire procedure usually takes only minutes, and the patient goes home the same day.
See Sacroiliac (SI) Joint Injections
The following outlines the typical injection procedure:
- After informed consent has been obtained, the patient lies face down on his or her stomach on the radiography table. A pillow might be placed under the hips for patient comfort.
- The patient's vitals (e.g. pulse rate and blood pressure) are monitored throughout the procedure.
- Depending on the physician and the patient's preference, an intravenous line may be inserted to deliver medication to help the patient relax.
- To maintain sterility, the skin overlying the sacroiliac joint injection is cleansed using an iodine based solution (e.g. Povidine-Iodine) or an alcohol-based antiseptic (e.g. chlorhexidine 0.5% in 70% alcohol). Sterile gloves are used throughout the entire injection procedure.
- For the patient's comfort, the needle insertion site is often numbed using local anesthetic. Once the needle enters the sacroiliac joint under fluoroscopy guidance, contrast - 'dye' that shows up under X-ray - is injected to verify needle placement within the sacroiliac joint and to verify spread of solution within the joint.
- Once the needle has been guided into the joint successfully, diagnostic and/or therapeutic medications are injected into the joint.
- Two types of medications are typically injected:
- A local anesthetic (usually lidocaine or bupivacaine) is typically injected into the joint with the goal of determining immediate pain relief to confirm the sacroiliac joint as the source of the patient's pain. This solution is used for a diagnostic sacroiliac joint injection.
- An anti-inflammatory medication (usually a corticosteroid) may help reduce inflammation within the joint, which in turn could help alleviate the pain over a longer period of time (typically for several months, up to a year). This solution is injected for a therapeutic sacroiliac joint injection.
This is a paid sponsorship by AstraZeneca. The content was developed by ONS and Margaret Barton-Burke, RN, FAAN, independently of AstraZeneca.
Large-volume (≥ 3 ml) intramuscular (IM) injections may not be administered often, and oncology nurses can be unfamiliar with best practices. A study found that only 32% of gluteal injections were administered into the desired IM target. This could lead to the drug being administered subcutaneously or near major nerves and blood vessels, potentially decreasing the treatment’s efficacy.
Faslodex® (fulvestrant), a selective estrogen receptor degrader indicated for advanced breast cancer as monotherapy or in combination with palbociclib, requires large-volume IM injections administered on days 1, 15, and 29 of each treatment cycle, then once monthly at 500 mg per dose. Fulvestrant packages contain two prefilled syringes of 250 mg/5 ml and 21-gauge, 1.5-inch general purpose SafetyGlide™ hypodermic needles. Each IM injection must be administered slowly (over one to two minutes) at two separate gluteal injection sites.
The proper method of administration of fulvestrant for IM use is described in the fulvestrant prescribing information:
- Remove glass syringe barrel from tray and check that it is not damaged.
- Remove perforated patient record label from syringe.
- Inspect drug product in glass syringe for any visible particulate matter or discoloration prior to use, and discard if particulate matter or discoloration is present.
- Peel open the safety needle outer packaging.
- Hold the syringe upright on the ribbed part. With the other hand, take hold of the cap and carefully tilt cap back and forth (DO NOT TWIST CAP) until the cap disconnects for removal.
- Pull the cap off in a straight, upward direction. DO NOT TOUCH THE STERILE SYRINGE TIP (Luer-Lok).
- Attach the safety needle to the syringe tip (Luer-Lok). Twist needle until firmly seated. Confirm that the needle is locked to the Luer connector before moving or tilting the syringe out of the vertical plane to avoid spillage of syringe contents.
- Pull shield straight off needle to avoid damaging needle point.
- Remove needle sheath.
- Expel excess gas from the syringe (a small gas bubble may remain).
- Administer intramuscularly slowly (1-2 minutes/injection) into the buttock (gluteal area). For user convenience, the needle “bevel up” position is orientated to the lever arm.
- After injection, immediately activate the lever arm to deploy the needle shielding by applying a single-finger stroke to the activation-assisted lever arm to push the lever arm completely forward. Listen for a click. Confirm that the needle shielding has completely covered the needle. Always activate away from self and others.
- Discard the empty single-use syringe into an approved sharps collector in accordance with applicable regulations and institutional policy.
- Repeat steps one through 13 for the second syringe.
- Traditionally, nurses have been trained to inject large volumes into the dorsogluteal site; however, the ventrogluteal site is evolving as a safer IM injection site (see TABLE 1 for an overview of both methods).
Nurses may also consider the Z-track method. See FIGURE 1 for more information.
- Consider the Z-track technique to reduce pain and prevent dispersion of medication into subcutaneous tissue.
- The Z-track method has been used to administer large-volume IM injections to reduce pain and subcutaneous tissue dispersion.
- Using the Z-track technique for IM injections prevents leakage of the medication into subcutaneous tissues and decreases the likelihood of localized irritation.
- Pull or push the skin 2–3 cm away from the injection site with the nondominant hand.
- Pierce the skin at 90° and depress the plunger slowly. If resistance occurs, pause then resume depressing the plunger.
- Withdraw the needle, then release the skin.
Fulvestrant is associated with injection-site pain, including sciatica, neuralgia, neuropathic pain, and peripheral neuropathy. Steps to minimize injection-site reactions include the following.
- Identifying bony anatomical landmarks and ensuring proper patient positioning offers a safe and effective means of IM delivery.
- Rotation of injection sites should be considered with repeated monthly injections.
- Use manual pressure before needle insertion to stimulate nerve endings and reduce sensory input during injection.
- Fulvestrant is highly viscous and passively warming to room temperature for 30 minutes before use has been suggested in the nursing literature. Alternatively, slowly rolling fulvestrant between the hands can minimize viscosity.
- Administer injections at a slow rate (over one to two minutes per injection).
- In patients with excessive subcutaneous fat, a 90° angle should be used to avoid injecting subcutaneously (see FIGURE 2).
- Be observant for factors that may increase the risk of bruising or bleeding (e.g., thrombocytopenia or anticoagulant use).
- Other steps to minimize injection-site reactions include the use of warm compresses and topical anesthetics.
Ongoing education regarding side effect recognition and management is important to help maintain patient quality of life and educate patients on queries such as how the drug will be injected, how often it will be administered, whether it will hurt, how they will feel the next day, and whether they will have injection-site pain.
An Interview With Margaret Barton-Burke, PhD, RN, FAAN
Q: A study cited in the poster noted that only 32% of intended gluteal injections were administered into the desired IM target. Do you find that this is a concern in the nursing community?
A: I would say absolutely, but specifically, this study reported gender findings and IM injections in women were found to be given more often into subcutaneous tissue. Women being given fulvestrant may not be getting their complete dose if the IM technique is not correct.
From a nursing perspective, it really begs the question, “How many patients are really getting fulvestrant administered in the muscle or subcutaneous tissue?” Nurses do not give IM injections frequently. However, for those that are required, are we giving these injections using proper technique?
Q: Do you often find that oncology nurses are unfamiliar with injection best practices?
A: I would tend to say no. Nurses are used to giving injections of all sorts and in a variety of ways. However, if a staff nurse is new to oncology, he or she may need to have a refresher on how to give an IM injection. Gail M. Wilkes, RN, MS, AOCN®, an independent oncology nurse consultant in Kilauea, HI, and I write a book every year called The Oncology Nursing Drug Handbook, and in that handbook, under fulvestrant, we recommend a Z-track technique. That is something you might learn in school but you might not use frequently because it is not a common way of giving an IM injection. In oncology, there is not much concern with unfamiliarity with injections, but more so with the type of injection
Q: Are there any other best practices that you recommend for these kinds of injections?
Smali Files
A: Best practices in the poster and manufacturer guidelines suggest splitting the dosage into two injections and administering into the gluteal muscle This is good practice both from a nursing and a patient perspective.
Q: What are the challenges nurses face when managing a patient who requires an IM injection therapy?
A: In general, the challenges are to be comfortable with giving an IM injection and to make sure that where you are placing the injection is into the gluteal muscle, avoiding the sciatic nerve. It is also important to consider our patient population, who tend to be at risk for bleeding. Being aware of the platelets counts and/or other laboratory findings are important prior to giving an IM injection. It is also important to be aware that these injections have the potential to be administered directly into a vein, and that is the main reason you check for placement by pulling back on the syringe when giving an IM injection. This should be done for all injections.
Q: What advice would you give to nurses to keep on top of education and updates surrounding injection best practices?
A: I am going to put on my ONS past president’s hat for a moment. ONS has a position statement that speaks to ongoing learning. After school or orientation, nurses do not stop learning, and that is the whole notion behind certification and keeping up your education.
Now I will put on my Memorial Sloan-Kettering Cancer Center hat. We have mandatory trainings yearly, and this is probably true for every hospital. Annually, I must complete trainings, and I had many trainings to complete initially when I came to the institution.
If a nurse has not given an IM injection in a while, he or she needs to say, “I have not given an IM injection for a while.” It is a clinical humility to admit when someone requires assistance. I would want, probably need, someone to walk me through the procedure. It does not matter how much education you have; my education has gone beyond the clinical area, and I think it is important to be safe in your practice. I would also read the drug information prior to administration.
I think nurses have an opportunity to conduct research and partner with other departments in the institution to replicate the Chan et al. study. We could corroborate or refute the findings from the Chan et al. study to gain the evidence for practice. We are all trying to use evidence-based practice.
Smali Comment
Q: Can you give an overview of the pros and cons of using an IM injection therapy?
A: For the pros, you can give deep muscle injections with a larger volume and the drug is absorbed over time in an area that is rich with blood flow.
For the cons, depending on the size of the individual and where on the body the injection is given (i.e., into which muscle), we need to avoid the sciatic nerve and the large blood vessels. Also, in a cancer patient population, we tend not to give IM injections since our patients may have low platelets and a potential for bleeding.
Another concern about IM injections is the pain. It is not comfortable if you give a large amount of solution, 2.5 ccs or mls, into each gluteal muscle. Nurses may have to pay more attention to rubbing the muscle a little bit more than you normally would after you give the injection due to the injected volume.
The Chan et al. article noted that patients with a higher body mass index, which also equates to more body fat, may require a different length needle than what you would normally use for an IM injection. This article helped me think about IM injections in a completely different way.
The poster is well done. And not only that, it really points to some of the issues that I do not think we take seriously in oncology. I applaud the authors on their work.
Heather Vanderploeg, RN, OCN, BSN, CBCN, from AstraZeneca, and co-authors presented this information during a poster session at the ONS 42nd Annual Congress in Denver, CO. The poster was titled “Review of Best Practices for Large-Volume Intramuscular Injection of Fulvestrant.”
To discuss the information in this article with other oncology nurses, visit the ONS Communities.
To report a content error, inaccuracy, or typo, email pubONSVoice@ons.org.
